Our Products
Others Services
Defol 6 ( Deflazacort 6 mg Tablets )
Additional Details
Defol 6mg Tablet belongs to a group of medicines called steroids. It is used for treatment of various diseases and conditions such as allergic conditions, asthma, cancer, rheumatic disorder, and skin and eye disorders.
Defol 6mg Tablet works by inhibiting the release of substances that cause swelling or by changing how the immune system works. It can be taken in an empty stomach or after food. Taking the medicine regularly at the right times increases its effectiveness. It is important to keep taking the medicine regularly until your doctor tells you it is safe to stop.
Taking this medicine can cause few common side effects such as increased appetite, frequent urge to urinate, facial swelling, and abnormal hair growth. If any of these side effects bothers you, let your doctor know.
Defol 6mg Tablet can make it harder for you to fight off infections. Tell your doctor if you have any signs of infection such as a fever or sore throat. Before taking the medicine, you should let your doctor know of all the other medicines you are taking. Pregnant and breastfeeding women should consult their doctors before taking the medicine.
Zopin ( Permethrin Lotion 5 % )
Additional Details
This medication is for use on the skin only. Apply this medication as soon as possible after it is prescribed. Apply the medicine from your head to the soles of your feet, including under your nails and in skin folds such as between the toes, as directed. Massage the cream into the skin. Do not use more medication than prescribed. Wash off the cream after 8-14 hours by showering or taking a bath.
Avoid getting the cream into your eyes, nose, mouth, or vagina. If the medication gets in your eyes, flush the eyes with plenty of water. Consult your doctor if irritation persists.
Symptoms of scabies include an intense itching that is usually worse at bedtime. You may also see small, fine, wavy lines on the skin with a tiny insect at the end (a burrow). Burrows are usually found on finger/toe webs, wrists, elbows, armpits, belt line, lower buttocks, female nipples, or male genitals. Even if permethrin kills all the scabies, the dead mites can still make you itch for up to 4 weeks after treatment. Ask your doctor about other medications that may be used to soothe the itching. Inform your doctor if your condition persists or worsens 2 weeks after treatment. Your doctor may need to look for living mites and recommend more treatment.
Silverpin - Plus ( Sliver Sulfadiazine Chlorhexidine Gluconate )
Additional Details
This medication is for use on the skin only. Avoid using this medication around your eyes unless directed to do so by your doctor.
Your health care professional will clean and remove the dead tissue from the wound to help the healing process.
Apply this medication to the wound using sterile technique (such as wearing sterile gloves and using sterile application tools), as directed by your doctor, usually 1 to 2 times daily. The layer of medication should be about one-sixteenth of an inch (1-2 millimeters) thick or as directed. The wound should be covered with the cream at all times. Dressings may be applied over the cream, but only if needed. If some of the cream rubs off the wound, reapply it immediately. The cream should also be reapplied immediately after hydrotherapy.
Treatment usually continues until the wound is completely healed or until the site is ready for skin grafting.
Cotiwin ( HYDRO CORTISONE )
Additional Details
HYDRO CORTISONE
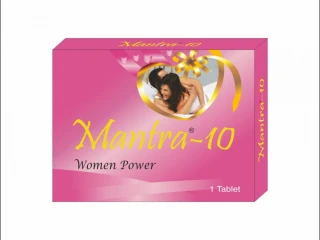
Mantra - 10
Additional Details
WOMEN'S HEALTH, WOMEN’S SEXUAL ENHANCEMENTTAGS: BENEFITS OF TADALAFIL 10MG TABLET, BUY TADALAFIL 10MG TABLET ONLINE, MANTRA 10 TABLET, MANTRA 10MG TABLET, ONLINE TADALAFIL 10MG TABLET, ONLINE WOMEN SEX POWER TABLET, TADALAFIL 10MG TABLET PRICE, TADFIL 10MG TABLET, USES OF TADALAFIL 10MG TABLET, WOMEN SEX POWER TABLET
Beta - Fort ( Betamethasone Tablets 1.0 mg )
Additional Details
The dose used will depend on the disease, its severity and the clinical response obtained. The following regimens are for guidance only. Divided dosage is usually employed.
Short term treatment:
2-3mg daily for the first few days, then reducing the daily dose by 250 or 500mcg (0.25 or 0.5mg) every two to five days, depending upon the response.
Rheumatoid arthritis:
500mcg (0.5mg) to 2mg daily. For maintenance therapy the lowest effective dosage is used.
1.5 to 5mg daily for one to three weeks, then reducing to the minimum effective dosage. Larger doses may be needed for mixed connective tissue diseases and ulcerative colitis.
Paediatric population:
A proportion of the adult dosage may be used (e.g. 75% at 12 years, 50% at 7 years and 25% at 1 year) but clinical factors must be given due weight (see section 4.4).
Method of Administration: Oral
4.3 Contraindications
Hypersensitivity to the active substance or to any of the excipients listed in section 6.1.
Systemic infections, unless specific anti-infective therapy is employed.
4.4 Special warnings and precautions for use
A patient information leaflet should be supplied with this product.
Undesirable effects may be minimised by using the lowest effective dose for the minimum period and by administering the daily requirement as a single morning dose, or whenever possible as a single morning dose on alternate days. Frequent patient review is required to appropriately titrate the dose against disease activity (see “Posology and Method of Administration”).
Caution is advised with the use of corticosteroids in patients who have suffered a recent myocardial infarction because of the risk of myocardial rupture.
Caution is advised on the use of corticosteroids in patients with hypothyroidism or myasthenia gravis.
Suppression of the inflammatory response and immune function increases the susceptibility to infections and their severity. The clinical presentation may often be atypical and serious infections such as septicaemia and tuberculosis may be masked and may reach an advanced stage before being recognised.
Chickenpox is of particular concern since this normally minor illness may be fatal in immunosuppressed patients. Patients (or parents of children) without a definite history of chickenpox should be advised to avoid close personal contact with chickenpox or herpes zoster and if exposed they should seek urgent medical attention. Passive immunisation with varicella zoster immunoglobulin (VZIG) is needed by exposed non-immune patients who are receiving systemic corticosteroids or who have used them within the previous 3 months; this should be given within 10 days of exposure to chickenpox. If a diagnosis of chickenpox is confirmed, the illness warrants specialist care and urgent treatment. Corticosteroids should not be stopped and the dose may need to be increased.
Live vaccines should not be given to individuals with impaired immune responsiveness. The antibody response to other vaccines may be diminished.
Patients should be advised to take particular care to avoid exposure to measles and to seek immediate medical advice if exposure occurs. Prophylaxis with intramuscular normal immunoglobulin may be needed.
Adrenal suppression:
Adrenal cortical atrophy develops during prolonged therapy and may persist for years after stopping treatment.
In patients who have received more than physiological doses of systemic corticosteroids (approximately 1mg betamethasone or equivalent) for greater than 3 weeks, withdrawal should not be abrupt. How dose reduction should be carried out depends largely on whether the disease is likely to relapse as a dose of systemic corticosteroids is reduced. Clinical assessment of disease activity may be needed during withdrawal. If the disease is unlikely to relapse on withdrawal of systemic corticosteroids but there is uncertainty about hypothalamic-pituitary-adrenal (HPA) suppression, the dose of systemic corticosteroid may be reduced rapidly to physiological doses. Once a daily dose equivalent to 1mg betamethasone is reached, dose reduction should be slower to allow the HPA-axis to recover.
Abrupt withdrawal of systemic corticosteroid treatment, which has continued up to 3 weeks is appropriate if it is considered that the disease is unlikely to relapse. Abrupt withdrawal of doses of up to 6mg daily of betamethasone, or equivalent for 3 weeks is unlikely to lead to clinically relevant HPA-axis suppression, in the majority of patients. In the following patient groups, gradual withdrawal of systemic corticosteroid therapy should be considered even after courses lasting 3 weeks or less:
• Patients who have had repeated courses of systemic corticosteroids, particularly if taken for greater than 3 weeks,
• When a short course has been prescribed within one year of cessation of long-term therapy (months or years),
• Patients who have reasons for adrenocortical insufficiency other than exogenous corticosteroids therapy,
• Patients receiving doses of systemic corticosteroid greater than 6mg daily of betamethasone (or equivalent),
• Patients repeatedly taking doses in the evening.
During prolonged therapy any intercurrent illness, trauma or surgical procedure will require a temporary increase in dosage; if corticosteroids have been stopped following prolonged therapy they may need to be temporarily re-introduced.
Special precautions
Particular care is required when considering the use of systemic corticosteroids in patients with the following conditions and frequent patient monitoring is necessary.
A. Osteoporosis (post-menopausal females are particularly at risk).
B. Hypertension or congestive heart failure.
C. Existing or previous history of severe affective disorders (especially previous steroid psychosis).
D. Diabetes mellitus (or a family history of diabetes).
E. History of tuberculosis.
F. Glaucoma (or a family history of glaucoma).
G. Previous corticosteroid-induced myopathy.
H. Liver failure - blood levels of corticosteroid may be increased, (as with other drugs which are metabolised in the liver).
I. Renal insufficiency.
J. Epilepsy.
K. Peptic ulceration.
Patients should carry 'steroid treatment' cards which give clear guidance on the precautions to be taken to minimise risk and which provide details of prescriber, drug, dosage and the duration of treatment.
Patients/and or carers should be warned that potentially severe psychiatric adverse reactions may occur with systemic steroids (see section 4.8). Symptoms typically emerge within a few days or weeks of starting treatment. Risks may be higher with high doses/systemic exposure (see also section 4.5 pharmacokinetic interactions that can increase the risk of side effects), although dose levels do not allow prediction of the onset, type, severity or duration of reactions. Most reactions recover after either dose reduction or withdrawal, although specific treatment may be necessary. Patients/carers should be encouraged to seek medical advice if worrying psychological symptoms develop, especially if depressed mood or suicidal ideation is suspected. Patients/carers should also be alert to possible psychiatric disturbances that may occur either during or immediately after dose tapering/withdrawal of systemic steroids, although such reactions have been reported infrequently.
Particular care is required when considering the use of systemic corticosteroids in patients with existing or previous history of severe affective disorders in themselves or in their first degree relatives. These would include depressive or manic-depressive illness and previous steroid psychosis.
Visual disturbance
Visual disturbance may be reported with systemic and topical corticosteroid use. If a patient presents with symptoms such as blurred vision or other visual disturbances, the patient should be considered for referral to an ophthalmologist for evaluation of possible causes which may include cataract, glaucoma or rare diseases such as central serous chorioretinopathy (CSCR) which have been reported after use of systemic and topical corticosteroids.
Paediatric population
Corticosteroids cause dose-related growth retardation in infancy, childhood and adolescence, which may be irreversible. Treatment should be limited to the minimum dosage for the shortest possible time. In order to minimise suppression of the HPA axis and growth retardation, consideration should be given to administration of a single dose on alternate days.
Elderly
The common adverse effects of systemic corticosteroids may be associated with more serious consequences in old age, especially osteoporosis, hypertension, hypokalaemia, diabetes, susceptibility to infection and thinning of the skin. Close clinical supervision is required to avoid life-threatening reactions.
Excipients
Sodium
This medicine contains less than 1 mmol sodium (23 mg) per tablet, that is to say essentially 'sodium-free'. For a dose ranging between two to ten tablets (1000 to 5000 micrograms per dose), this medicine contains between 41.8 mg and 209 mg sodium (main component of cooking/table salt) in each dose. This is equivalent to 1.74% to 8.70% of the UK recommended maximum daily dietary intake of 2.4g sodium for an adult.
Sodium Benzoate
This medicine contains 6mg of sodium benzoate in each tablet. Sodium benzoate may increase jaundice (yellowing of the skin and eyes) in newborn babies (up to 4 weeks old).
4.5 Interaction with other medicinal products and other forms of interaction
Steroids may reduce the effects of anticholinesterases in myasthenia gravis, cholecystographic X-ray media and non-steroidal anti-inflammatory agents.
Rifampicin, rifabutin, carbamazepine, phenobarbitone, phenytoin, primidone, aminoglutethimide and ephedrine enhance the metabolism of corticosteroids; thus the corticosteroid therapeutic effect may be reduced.
The desired effects of hypoglycaemic agents (including insulin), anti-hypertensives and diuretics are antagonised by corticosteroids, and the hypokalaemic effects of acetazolamide, loop diuretics, thiazide diuretics and carbenoxolone are enhanced.
The efficacy of coumarin anticoagulants may be enhanced by concurrent corticosteroid therapy and close monitoring of the INR or prothrombin time is required to avoid spontaneous bleeding.
The renal clearance of salicylates is increased by corticosteroids and steroid withdrawal may result in salicylate intoxication.
The risk of hypokalaemia is increased with theophylline, ulcer healing drugs such as carbenoxolone and antifungals such as amphotericin B.
Increased toxicity may result if hypokalaemia occurs in patients on cardiac glycosides.
Ritonavir and oral contraceptives may result in increased plasma concentrations or corticosteroids.
The effect of corticosteroids may be reduced for 3-4 days after mifepristone.
The growth promoting effect of somatropin may be inhibited by corticosteroids.
An increase in the incidence of gastrointestinal bleeding may occur if NSAIDS are taken concomitantly with corticosteroids.
Corticosteroids may antagonise the effects of neuromuscular blocking drugs such as vecuronium.
Concurrent use of corticosteroids and fluoroquinolones may result in increased risk of tendon rupture.
Concomitant use of betamethasone with quetiapine may result in the increased metabolism of quetiapine and, depending on the clinical response, a higher dose of quetiapine may need to be considered.
Co-treatment with CYP3A inhibitors, including cobicistat-containing products, is expected to increase the risk of systemic side-effects. The combination should be avoided unless the benefit outweighs the increased risk of systemic corticosteroid side-effects, in which case patients should be monitored for systemic corticosteroid side-effects.
Corticosteroids may enhance the metabolism of tretinoin resulting in decreased levels of tretinoin.
4.6 Fertility, pregnancy and lactation
Pregnancy
The ability of corticosteroids to cross the placenta varies between individual drugs, however, betamethasone readily crosses the placenta. Administration of corticosteroids to pregnant animals can cause abnormalities of foetal development including cleft palate, intra-uterine growth retardation and effects on brain growth and development. There is no evidence that corticosteroids result in an increased incidence of congenital abnormalities, such as cleft palate/lip in man. However, when administered for prolonged periods or repeatedly during pregnancy, corticosteroids may increase the risk of intra-uterine growth retardation. Hypoadrenalism may, in theory, occur in the neonate following prenatal exposure to corticosteroids but usually resolves spontaneously following birth and is rarely clinically important. Myocardial hypertrophy and gastroesophageal reflux have been reported in association with in-utero exposure to betamethasone.
As with all drugs, corticosteroids should only be prescribed when the benefits to the mother and child outweigh the risks. When corticosteroids are essential however, patients with normal pregnancies may be treated as though they were in the non-gravid state. Patients with pre-eclampsia or fluid retention require close monitoring.
Betamethasone, systemically administered to a woman during pregnancy may result in a transient suppression of the foetal heart rate parameters and biophysical activities that are widely used for the assessment of foetal well – being. These characteristics can include a reduction in foetal breathing movements, body movements and heart rate.
Breast-feeding
Corticosteroids may pass into breast milk, although no data are available for betamethasone. Infants of mothers taking high doses of systemic corticosteroids for prolonged periods may have a degree of adrenal suppression.
4.7 Effects on ability to drive and use machines
Not relevant
4.8 Undesirable effects
The incidence of predictable undesirable effects, including hypothalamic-pituitary-adrenal (HPA) axis suppression correlates with the relative potency of the drug, dosage, timing of administration and the duration of treatment. (see section 4.4)
Not known: frequency cannot be estimated from the available data
Zitarax ( Hydroxyzine HCl. 10 mg./ 5 ml. )
Additional Details
Primary skeletal muscle relaxation has been demonstrated experimentally. Bronchodilator activity, and antihistaminic and analgesic effects have been demonstrated experimentally and confirmed clinically. An antiemetic effect, both by the apomorphine test and the veriloid test, has been demonstrated.
Pharmacological and clinical studies indicate that hydroxyzine in therapeutic dosage does not increase gastric secretion or acidity and in most cases has mild antisecretory activity.
Hydroxyzine is rapidly absorbed from the gastrointestinal tract and hydroxyzine hydrochloride's clinical effects are usually noted within 15 to 30 minutes after oral administration.
Medication Guide
PATIENT INFORMATION
No information provided. Please refer to the PRECAUTIONS section.
FROM WebMD Logo
Healthy Resources
Tips to Keep Your Brain Healthy
What's Waking You Up Over and Over?
Featured Centers
Good and Bad Foods for Psoriasis
Video: Getting Personal on Life With MS
Health Solutions From Our Sponsors
Shot-Free MS Treatment
Your Child and COVID-19
FDA Logo
REPORT PROBLEMS TO THE FOOD AND DRUG ADMINISTRATION
You are encouraged to report negative side effects of prescription drugs to the FDA. Visit the FDA MedWatch website or call 1-800-FDA-1088.
Health Solutions From Our Sponsors
Penis Curved When Erect
Could I have CAD?
Treat Bent Fingers
Discover hATTR Symptoms
Tired of Dandruff?
Treat HR+, HER2- MBC
CONTINUE SCROLLING FOR RELATED SLIDESHOW
Pill Identifier Tool Quick, Easy, Pill Identification
Drug Interaction Tool Check Potential Drug Interactions
Pharmacy Locater Tool Including 24 Hour, Pharmacies
Related Drugs
Allegra Allegra-D Allegra-D 24 Hour Benadryl Benadryl Injection Clarinex Clarinex-D 12hr Clarinex-D 24hr Claritin Claritin D Rhinocort Aqua Sudafed Vistaril Zyrtec Zyrtec-D
Health Resources
Allergy (Allergies) Eczema Interstitial Cystitis (IC) and Painful Bladder Syndrome (PBS) Sleep Disorders (How to Get a Good Night's Sleep) Panic Attacks (Panic Disorder) FAQs Posttraumatic Stress Disorder (PTSD) FAQs
Related Supplements
Dmso (Dimethylsulfoxide) Lactobacillus Melatonin Tyrosine Whey Protein
Drug Comparison
Atarax vs. Ativan Benadryl vs. Atarax Benadryl vs. Zyrtec Claritin vs. Claritin D Vistaril vs. Atarax
ATARAX USER REVIEWS
Monokit Shampoo ( Ketoconazole Zpto Shampoo )
Additional Details
Ketoconazole is a synthetic antifungal drug used to prevent and treat skin and fungal infections, especially in immunocompromised patients such as those with AIDS. Ketoconazole is sold commercially as an anti-dandruff shampoo, topical cream, and oral tablet, under the trademark name Nizoral by Johnson & Johnson. Ketoconazole is very lipophilic, which leads to accumulation in fatty tissues. The less toxic and more effective triazole compounds fluconazole and itraconazole have largely replaced ketoconazole for internal use. Ketoconazole is best absorbed at highly acidic levels, so antacids or other causes of decreased stomach acid levels will lower the drug's absorption when taken orally.
Pharmacodynamics
Pharmacokinetics
Ketoconazole interferes with biosynthesis of triglycerides and phopholipids by blocking fungal cytochrome P450, thus altering cell membrane permeability in susceptible fungi. It also inhibits other fungal enzymes resulting in the accumulation of toxic concentrations of hydrogen peroxide.
© Terrace Pharmaceuticals Pvt Ltd. All Rights Reserved
Developed and Managed by Bizz Digital Solutions
